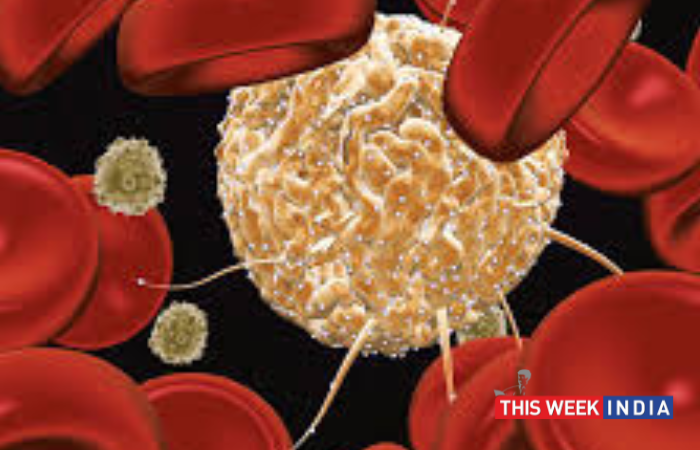
Bangalore, June 16, 2022: There are as many as 2.5 million carrier of the gene (Hemoglobin AS) in India that can lead to sickle cell disease, with more than 1,25,000 actual patients spread across the country, with a much higher incidence in the tribal belt of the country. Sickle cell disease is associated with a significant risk of morbidity and premature mortality, especially among children. While in the west, a child receiving comprehensive care in high-resource settings has an estimated 99% survival into adulthood. However, in India, according to an ICMR study, about 20 per cent of children with sickle disease died by the age of two, and 30 per cent children with Sickle Cell Disease die before they reach adulthood.
Dr. Biju George, Professor & Head, Department of Haematology at CMC Vellore, “People with Sickle Cell Disease, may beat a risk of progressive organ damage, impaired quality of life, considerable morbidity in childhood, and risk of premature mortality in adulthood [median survival of 58 years]. Sickle Cell disease patients who are undergoing regular life-long blood transfusions, have the best chance of survival and cure with a blood stem cell transplant. This transplant can come from a sibling or a family member. However, there is only a 30% chance of finding a “matched” sibling donor in the same family. The remaining 70% patients look for a matching donor through a stem cell registry or donor center- a database of voluntary donors between the age group of 18 to 50 years.”
Dr. Govind Eriat Nair, Consultant Hematology Hemato-Oncology and Bone Marrow Transplant Gleneagles Global BGS Hospital, Bengaluru, “If there is a fully HLA matched donor in the family, there is a 90-95% chance of cure with higher cure rates in younger children of below 12 years of age. However, due to underrepresentation of Indians in the global donor data pool, patients are unable to find a match on time. Also, the awareness about the disease is less, need of the hour is to raise the social awareness about this disease. Genetic counseling and newborn screening are the way forward. Effects of endogamy, consanguinity and role prenatal counseling needs to be addressed in primary screening.”
DKMS BMST Foundation India is a non-profit organization dedicated to the fight against blood cancer and other blood disorders, such as thalassemia and sickle cell disease. The organization aims to give every blood disorder patient in need a second chance at life.
To mark World Sickle Cell Day, Patrick Paul, CEO, DKMS BMST Foundation India said, “Sickle cell has variance and only the severe form needs a stem cell transplant. An early transplant can help patient with severe Sickle cell disease from organ damage. With rising cases in India, it is the need of the hour that stem cell transplants are made available to more patients to save lives. But due to the misconceptions and lack of awareness about blood stem cell donation, Indians are highly underrepresented in the global donor pool. This situation can only be changed by recruiting many more potential blood stem cell donors from the Indian ethnicity.”
The success of a stem cell transplant depends of donor’s HLA (Human Leukocyte Antigen) matching the patient. The body’s immune system has proteins known as HLA to distinguish cells that belong to the body from those that do not. DKMS-BMST helps in unrelated donor transplant process which includes enrolling and counselling the donors, get their HLA typing done, facilitate search of the donors and later facilitate the blood stem cell collection and the transplant. So, far DKMS-BMST has registered over 60,000 potential donors and have helped 60 patients with second chance at life.
Register as a potential blood stem cell donor:
Healthy individuals between 18-50 years of age can register at: dkms-bmst.org/register
All it takes is five minutes of your time and a simple 3 step process:
Step 1: Visit the site, fill up an online form and you will receive a DIY swab kit at home.
Step 2: Once you receive the swab kit, fill out the consent form and take a tissue sample from the inside of your cheeks with 3 cotton swabs provided in the kit.
Step 3: Send back your swab sample in the pre-paid envelope provided.
DKMS laboratory will then analyze your tissue type and your details will be available in the global search for blood stem cell donors. If you do come up as a suitable donor, DKMS-BMST will get in touch with you straight away. Once you come up as a match, blood stem cells will be obtained from the bloodstream using a procedure called Peripheral Blood Stem Cell Collection, which is similar to a blood donation wherein only your stem cells are taken. This is a safe, non-surgical outpatient procedure.